Training on state-specific health insurance regulations with AI call analytics
-
Bella Williams
- 10 min read
Training on state-specific health insurance regulations is crucial for customer-facing teams in the healthcare sector. With the complexities of varying state laws, leveraging AI call analytics can significantly enhance training effectiveness. By analyzing real-time call data, organizations can identify knowledge gaps among agents, ensuring they are well-versed in the specific regulations that apply to their state. This approach not only streamlines compliance training but also improves overall customer interactions by providing agents with the insights needed to address inquiries accurately and efficiently. As we delve into this topic, we will explore how AI-powered call analytics can transform training programs, enhance agent performance, and ultimately lead to better customer experiences in the health insurance landscape.
State-Specific Health Insurance Regulations Explained
Training on state-specific health insurance regulations is essential for customer-facing teams in the healthcare sector, particularly given the complexities and variations in laws across different states. By utilizing AI-powered call analytics, organizations can significantly enhance the effectiveness of their training programs. This technology allows for the real-time analysis of customer interactions, identifying knowledge gaps among agents and ensuring they are well-equipped to handle inquiries related to specific state regulations.
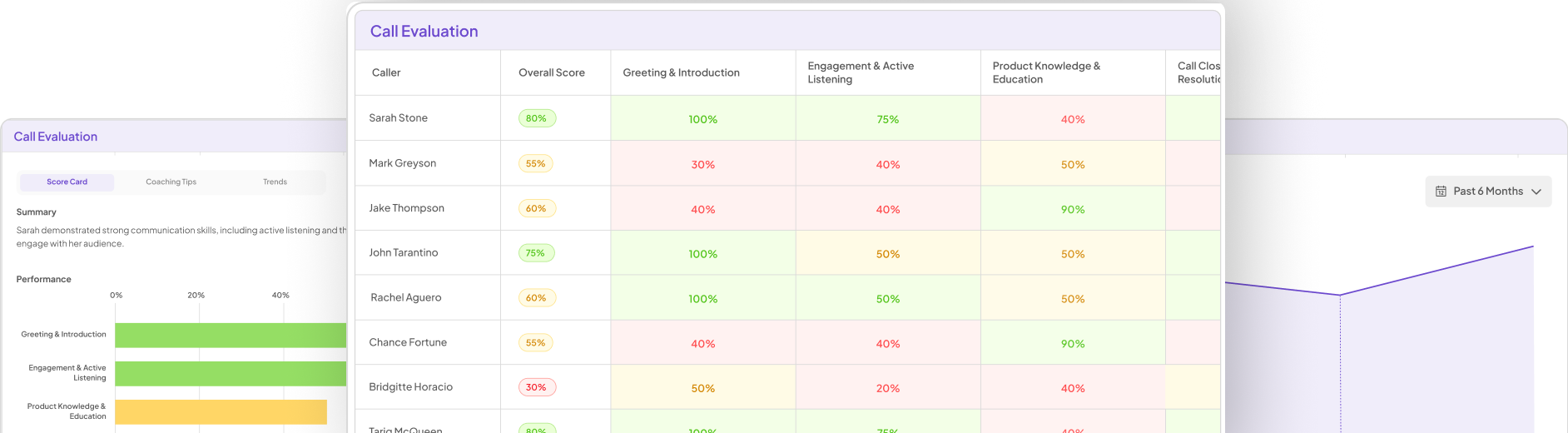
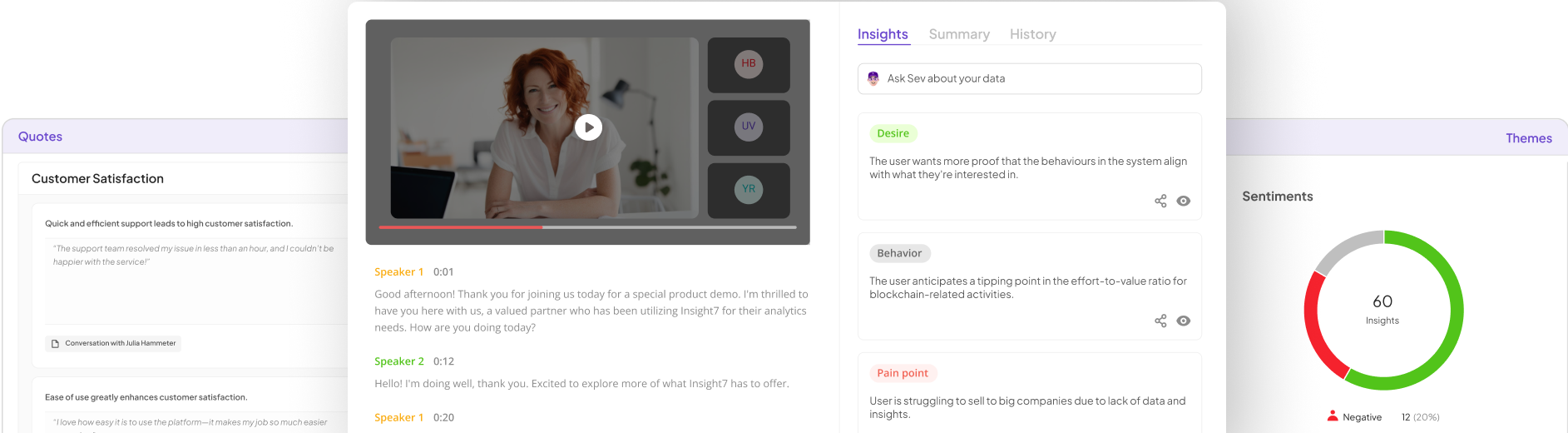
AI call analytics platforms, such as Insight7, automatically evaluate customer conversations, scoring interactions against custom quality criteria. This capability enables organizations to detect sentiment, empathy, and resolution effectiveness, providing a comprehensive view of agent performance. By analyzing these interactions, leaders can uncover recurring customer pain points and sentiment trends, which are crucial for refining training programs.
One of the core advantages of AI call analytics is its ability to deliver consistent and unbiased quality assurance insights across teams. This consistency is vital when training agents on the nuances of state-specific regulations, as it ensures that all team members receive the same level of information and guidance. Additionally, the platform's multilingual support allows organizations to evaluate global conversations accurately, catering to diverse customer bases and regulatory environments.
Coaching and performance management are also enhanced through AI-driven insights. By generating actionable coaching recommendations from real conversations, organizations can track agent performance and improvement over time. This targeted approach helps identify skill gaps and suggests specific coaching interventions, ensuring that agents are not only compliant with regulations but also proficient in delivering high-quality customer service.
Moreover, AI call analytics can surface upsell and cross-sell opportunities during support interactions. By detecting these moments in real-time, organizations can train their agents to recognize and act on potential revenue opportunities while addressing customer needs. This dual focus on compliance and revenue generation is particularly beneficial in the competitive health insurance landscape.
The integration of AI call analytics into training programs also streamlines the onboarding process for new agents. By providing immediate access to relevant insights and training materials, organizations can reduce the time it takes for new hires to become proficient in state-specific regulations. This efficiency not only enhances agent confidence but also improves the overall customer experience.
In summary, leveraging AI-powered call analytics for training on state-specific health insurance regulations offers a transformative approach to compliance training. By utilizing real-time data to identify knowledge gaps, enhance coaching, and streamline onboarding, organizations can ensure their customer-facing teams are well-prepared to navigate the complexities of health insurance regulations. This not only leads to improved agent performance but also fosters better customer interactions, ultimately driving growth and satisfaction in the healthcare sector.
AI Call Analytics Tools for Compliance Training
Training on state-specific health insurance regulations with AI call analytics can significantly enhance compliance training for customer-facing teams. By leveraging AI-powered call analytics tools, organizations can analyze real-time customer interactions to identify knowledge gaps among agents regarding specific regulations. This approach ensures that agents are well-equipped to handle inquiries accurately and efficiently, ultimately improving customer experiences.
AI call analytics platforms, like Insight7, automatically evaluate customer conversations, scoring them against custom quality criteria. This capability allows organizations to detect sentiment, empathy, and resolution effectiveness, providing a comprehensive view of agent performance. By uncovering recurring customer pain points and sentiment trends, leaders can refine training programs to better address the complexities of state-specific regulations.
Furthermore, AI-driven insights facilitate targeted coaching, helping agents improve their performance over time. This targeted approach ensures compliance with regulations while enhancing the quality of customer service. Additionally, AI call analytics can identify upsell and cross-sell opportunities during support interactions, enabling agents to act on potential revenue opportunities while addressing customer needs.
In summary, utilizing AI-powered call analytics for training on state-specific health insurance regulations offers a transformative approach to compliance training. By identifying knowledge gaps, enhancing coaching, and streamlining onboarding, organizations can ensure their customer-facing teams are well-prepared to navigate the complexities of health insurance regulations, leading to improved agent performance and better customer interactions.
Comparison Table
Training on state-specific health insurance regulations with AI call analytics is a game-changer for organizations aiming to enhance compliance training for customer-facing teams. By leveraging AI-powered call analytics tools, businesses can analyze real-time customer interactions to pinpoint knowledge gaps among agents regarding specific regulations. This ensures that agents are equipped to handle inquiries accurately and efficiently, ultimately improving customer experiences.
AI call analytics platforms, such as Insight7, automatically evaluate customer conversations, scoring them against custom quality criteria. This capability allows organizations to detect sentiment, empathy, and resolution effectiveness, providing a comprehensive view of agent performance. By uncovering recurring customer pain points and sentiment trends, leaders can refine training programs to better address the complexities of state-specific regulations.
Moreover, AI-driven insights facilitate targeted coaching, helping agents improve their performance over time. This ensures compliance with regulations while enhancing the quality of customer service. Additionally, AI call analytics can identify upsell and cross-sell opportunities during support interactions, enabling agents to act on potential revenue opportunities while addressing customer needs.
In summary, utilizing AI-powered call analytics for training on state-specific health insurance regulations offers a transformative approach to compliance training. By identifying knowledge gaps, enhancing coaching, and streamlining onboarding, organizations can ensure their customer-facing teams are well-prepared to navigate the complexities of health insurance regulations, leading to improved agent performance and better customer interactions.
Selection Criteria
Training on state-specific health insurance regulations with AI call analytics is a transformative approach that enhances compliance training for customer-facing teams. By utilizing AI-powered call analytics tools, organizations can analyze real-time customer interactions to identify knowledge gaps among agents regarding specific regulations. This ensures that agents are well-equipped to handle inquiries accurately and efficiently, ultimately improving customer experiences.
AI call analytics platforms like Insight7 automatically evaluate customer conversations against custom quality criteria, allowing organizations to detect sentiment, empathy, and resolution effectiveness. This comprehensive view of agent performance helps leaders refine training programs to address the complexities of state-specific regulations effectively.
Moreover, AI-driven insights facilitate targeted coaching, enabling agents to improve their performance over time while ensuring compliance with regulations. Additionally, AI call analytics can identify upsell and cross-sell opportunities during support interactions, allowing agents to address customer needs while capitalizing on potential revenue opportunities.
In summary, leveraging AI-powered call analytics for training on state-specific health insurance regulations not only identifies knowledge gaps but also enhances coaching and streamlines onboarding. This ensures that customer-facing teams are well-prepared to navigate the complexities of health insurance regulations, leading to improved agent performance and better customer interactions.
Frequently Asked Questions
Content for section: Frequently Asked Questions – comprehensive analysis and insights.