How to Audit Insurance Claims Calls With Transcript Tools
-
Bella Williams
- 10 min read
Claims Call Audit is an essential process in the insurance industry, ensuring that calls meet compliance standards and deliver quality service. Picture a world where every call is scrutinized with precision, helping agents refine their approach and enhance customer interactions. This systematic review of claims calls provides valuable insights into communication effectiveness, ensuring that agents convey information accurately and within regulatory guidelines.
Incorporating cutting-edge transcript tools can streamline this audit process significantly. By automating the identification of key phrases and compliance issues, insurers can focus on improving their performance rather than spending hours sifting through recordings. This not only elevates the quality of claims but also fosters a culture of accountability and continuous improvement among agents. Understanding the impact of a Claims Call Audit is the first step toward achieving excellence in customer service and operational efficiency.
Analyze & Evaluate Calls. At Scale.
Understanding the Importance of a Claims Call Audit
A Claims Call Audit plays a pivotal role in ensuring compliance and enhancing service quality in the insurance industry. By systematically evaluating call recordings, organizations can identify whether representatives adhere to established guidelines and regulations. This analysis helps pinpoint areas for improvement and ensures agents communicate essential information accurately and effectively.
Moreover, a claims call audit fosters accountability among staff. When employees know their calls are reviewed, they are more likely to follow scripts and guidelines meticulously. This focus not only enhances customer experience but also minimizes compliance risks associated with misleading or incorrect information. Ultimately, implementing a rigorous auditing process cultivates a culture of continuous improvement, leading to better service delivery and increased client trust.
Key Benefits of Auditing Insurance Claims Calls
Auditing insurance claims calls offers several key benefits that can significantly enhance the efficiency and compliance of claims handling. First, a Claims Call Audit helps ensure that agents adhere to regulatory guidelines, minimizing the risk of non-compliance. By analyzing interactions, insurers can identify potential compliance issues, thus safeguarding the organization from penalties and lawsuits. This proactive approach not only protects the company but also improves overall service quality.
Additionally, such audits facilitate performance evaluation and targeted training. By pinpointing areas where agents excel or struggle, organizations can tailor training programs to address specific needs, fostering a culture of continuous improvement. Furthermore, regular audits inspire confidence among clients, showcasing the commitment to high standards in service. In summary, implementing a Claims Call Audit enables organizations to enhance compliance, optimize agent performance, and ultimately deliver a superior customer experience.
Common Challenges in Claims Call Audits
Auditing insurance claims calls presents several challenges that can impede the effectiveness of the process. One major obstacle is the sheer volume of calls that need to be assessed, making it difficult to sift through and extract relevant information. This vast amount of data can overwhelm audit teams, resulting in critical details being overlooked. Additionally, maintaining consistency and objectivity in evaluations can prove challenging, as the subjective interpretation of call quality may vary among auditors.
Another significant challenge involves keeping up with compliance standards and changes in regulations. Call audits must accurately reflect these evolving requirements, which can impact the training and performance of staff. Inconsistencies in the audit process can lead to compliance risks and ultimately affect customer trust. To successfully navigate these challenges, organizations need tailored strategies and effective transcript tools that streamline the audit process while ensuring quality and compliance are maintained.
Extract insights from interviews, calls, surveys and reviews for insights in minutes
Step-by-Step Claims Call Audit Process
The Claims Call Audit process is vital for ensuring compliance and improving customer interactions. Begin this process by defining clear audit goals to guide your evaluation. This involves identifying key performance indicators, such as accuracy of information shared during calls, adherence to regulatory standards, and the overall customer experience. Setting these benchmarks will provide a solid foundation for your audit.
Next, it's essential to select appropriate transcript tools that facilitate a thorough analysis. Tools like Insight7 can enhance your ability to sort and analyze calls effectively. You may also consider alternatives such as Rev.com, Otter.ai, Sonix.ai, and Temi. Each tool offers unique features to help you extract insights from your calls. After selecting your tools, proceed to analyze the calls based on your established criteria. Document your findings meticulously to highlight areas for improvement. This organized approach will empower your team to address any compliance issues and enhance overall service quality.
Step 1: Setting Up the Audit Goals
Establishing clear audit goals is the foundational step in conducting a successful claims call audit. Begin by defining specific objectives that will guide the evaluation process. Consider what you want to achieve, such as compliance monitoring, quality assurance, or customer satisfaction assessment. By clarifying your goals, you set a benchmark against which all calls will be measured.
Next, it's crucial to identify the metrics and criteria that align with your objectives. For instance, if your goal revolves around compliance, you might focus on adherence to scripts, accuracy of information, and the management of customer inquiries. Establishing these parameters will ensure that the audit remains structured and focused, leading to actionable insights. By taking this initial step seriously, you enhance the effectiveness of the claims call audit process and improve overall outcomes.
Step 2: Selecting and Utilizing Transcript Tools
Selecting and utilizing transcript tools can greatly enhance the claims call audit process. These tools provide a method to transcribe recorded calls efficiently, ensuring you capture every detail for analysis. Begin by identifying tools that cater specifically to your needs, such as Rev.com, Otter.ai, or Sonix.ai. Each of these platforms offers unique features, including bulk transcription and insight generation, making them valuable resources for auditing insurance claims calls.
Once you've chosen a transcription tool, upload your call recordings for processing. This step will transform audio files into text, enabling thorough analysis of conversations for trends and patterns. Look for tools that allow you to extract key insights directly from transcripts, as this can streamline the auditing process significantly. By selecting the right transcript tools, you can ensure a more effective claims call audit, ultimately leading to better outcomes for your organization and clients.
Insight7
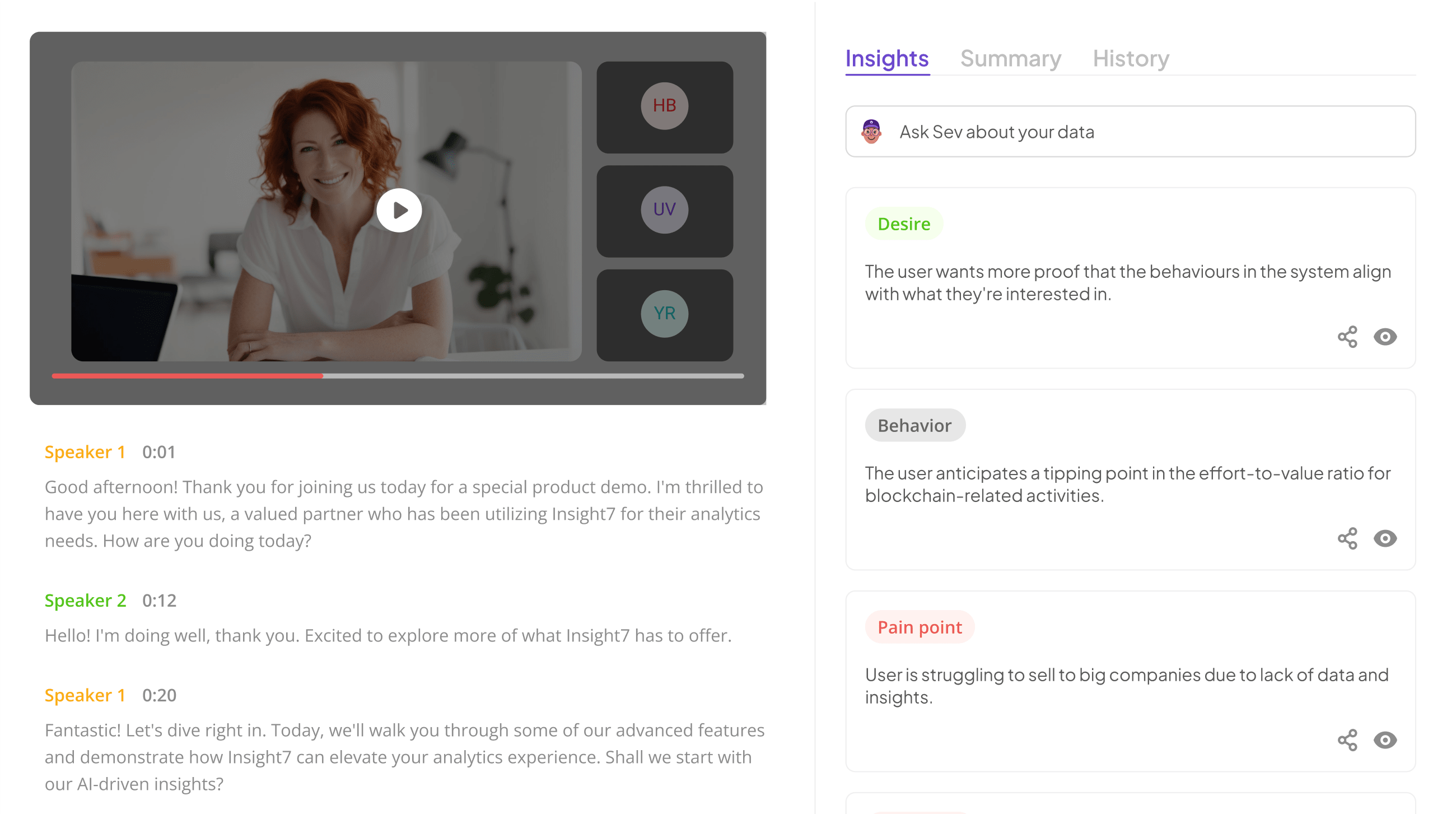
Utilizing transcript tools for insurance claims calls can significantly enhance the auditing process. Insight7 offers a streamlined platform designed to analyze customer conversations effectively, helping teams to identify key patterns and insights. By focusing on accuracy, the platform enables users to capture the essence of each interaction, laying the groundwork for informed decision-making regarding claims processes.
The benefits of employing Insight7 include improved efficiency in identifying customer needs and issues, along with the ability to adapt strategies based on real-time feedback. Additionally, the tool supports collaboration by centralizing insights, reducing the time spent on manual analysis. This efficiency allows insurance companies to respond swiftly to customer concerns and adjust their offerings as necessary, ultimately leading to enhanced customer satisfaction and loyalty.
- An overview and benefits of using Insight7 for claims auditing.
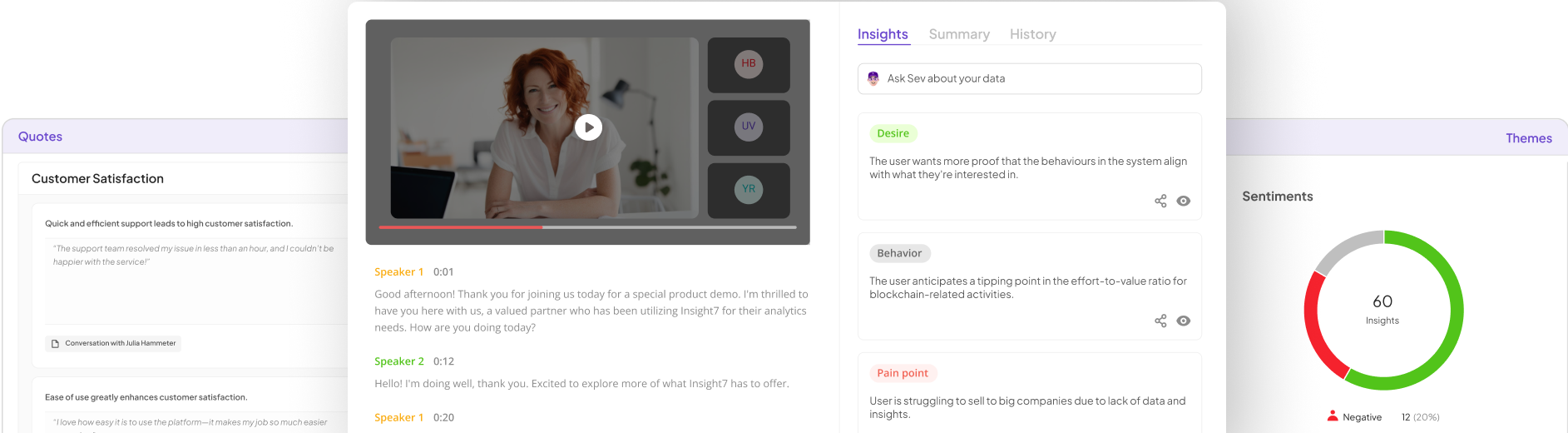
Using insight-driven technology can significantly enhance the claims auditing process. Insight7 offers intuitive tools designed to simplify claims call audits for insurance providers. The platform focuses on democratizing data access, allowing team members at all levels to engage in the auditing process. By providing straightforward interfaces, users can easily manage calls, analyze customer experiences, and identify friction points in real time.
One of the key benefits of using Insight7 is its ability to pull actionable insights from a multitude of calls with minimal effort. Users can access specific details like customer pain points and behaviors, which can be visualized in an easy-to-navigate format. This streamlined access to data facilitates a more comprehensive understanding of customer interactions, leading to improved service delivery and claims handling. By integrating these capabilities, organizations can enhance their auditing processes and drive better outcomes for both the business and its customers.
Additional Transcript Tools
When auditing insurance claims calls, utilizing additional transcript tools can significantly enhance the efficiency and depth of your analysis. These tools assist in transcribing audio recordings, making it easier to extract crucial insights from customer interactions. For instance, services like Rev.com, Otter.ai, Sonix.ai, and Temi provide reliable transcription options, ensuring you can focus on evaluating call content without the burden of manual transcription.
Each tool offers unique features that cater to different needs. Rev.com is known for its high accuracy, making it ideal for critical audits. Otter.ai provides real-time transcription and collaboration features, perfect for team evaluations. Sonix.ai allows users to easily search through transcripts, helping quickly identify relevant information. Lastly, Temi focuses on affordability, making it accessible for smaller teams. Exploring these additional transcript tools encourages a comprehensive and effective approach when conducting a claims call audit.
- Rev.com
When it comes to the process of claims call auditing, utilizing effective transcript tools enhances accuracy and efficiency. One significant player in this domain provides a user-friendly platform that allows insurance firms to transcribe calls seamlessly. These transcripts serve as pivotal references for evaluating customer interactions, enabling precise reviews and insightful analyses.
Such a tool is indispensable for realizing the full potential of a claims call audit. It helps in identifying trends, training gaps, and areas for customer service improvement. This results in better communication strategies and ultimately helps in fostering trust among clients. Through the power of transcriptions, organizations can transform individual customer conversations into valuable insights, leading to improved service quality and operational excellence. Adopting a reliable transcript tool ensures that audit processes become not only efficient but also more informed.
- Otter.ai
In the realm of auditing insurance claims calls, a reliable transcription tool plays a pivotal role in enhancing accuracy and efficiency. Otter.ai stands out among many tools, offering features tailored for effective claims call audits. By converting speech into text in real-time, it helps ensure that no crucial details are lost during conversations with clients. This functionality allows auditors to focus on analyzing the dialogue rather than frantically taking notes.
Another significant advantage of using Otter.ai is its powerful search capability. Users can quickly find specific keywords or phrases from calls, streamlining the audit process. This not only saves time but also boosts the overall quality of claims call audits. As teams strive to maintain high standards, employing transcription tools like Otter.ai can significantly improve the process of evaluating calls. Thus, it empowers insurance professionals to better coach their agents and enhance customer service.
- Sonix.ai
Using advanced transcript tools can significantly enhance the claims call audit process in the insurance industry. Among these tools, one particular solution stands out due to its user-friendly features and robust capabilities. For anyone involved in auditing insurance claims calls, harnessing efficient transcription technology is essential for reviewing and enhancing call quality.
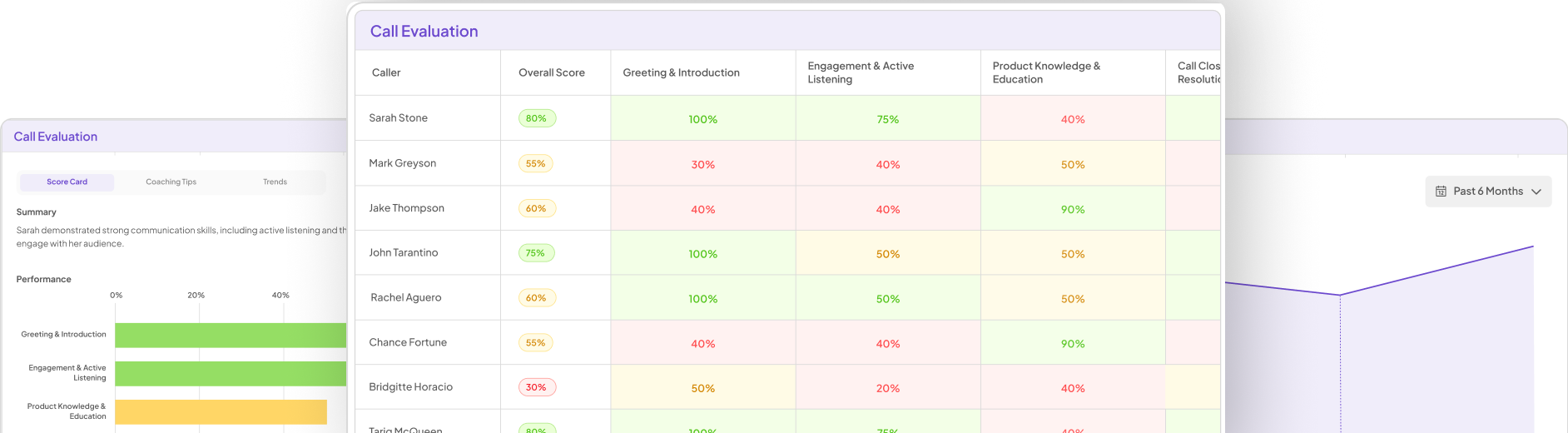
This tool enables users to accurately transcribe calls, helping auditors identify key patterns and insights across different interactions. Users can easily monitor agent performances, engagement levels, and compliance with guidelines, all of which are crucial in assessing the effectiveness of claims handling. The platform allows for the generation of detailed reports that provide a comprehensive overview of individual agent performance, facilitating targeted training and performance improvements.
With a focus on claims call audit processes, adopting such transcript technologies can streamline operations and deliver actionable insights to optimize the insurance claims experience.
- Temi
Temi is an invaluable tool for conducting a comprehensive claims call audit. It offers a streamlined way to record and transcribe calls, which enhances the efficiency of the auditing process. By converting spoken dialogue into written text, Temi allows auditors to meticulously examine conversations, ensuring compliance with standards and identifying areas for improvement. This ease of use means that team members can start analyzing claims calls without needing extensive training or technical support.
When utilizing Temi for claims call audits, it's essential to focus on specific aspects, such as adherence to compliance templates and assessing customer engagement. The structured format provided by Temi enables auditors to evaluate critical criteria effectively. Furthermore, the ability to highlight key quotes and themes from the transcripts facilitates a deeper understanding of call dynamics. By integrating Temi into your auditing process, you enhance your team's capability to provide actionable insights and improve overall performance in handling insurance claims.
Step 3: Analyzing and Reporting Findings
In the process of a Claims Call Audit, analyzing and reporting findings is crucial for understanding trends and patterns among calls. Begin by organizing call transcripts into a project that focuses on a specific time frame, such as monthly or quarterly evaluations. This approach allows you to systematically assess various aspects, from customer pain points to service delivery efficiency. Using analytical tools, you can identify recurring themes in the conversations that will guide your insights.
Once the data is organized, extract key findings and patterns. Calculate metrics, such as the percentage of calls that mention certain issues, to provide a quantitative basis for your analysis. Summarizing these insights into reports can highlight the most relevant points, ensuring that stakeholders understand the implications. Employ visualizations to illustrate customer journeys and pain points, making the information easily digestible. Ultimately, clear reporting of findings will facilitate improvements in call handling processes and enhance customer satisfaction.
Conclusion: Mastering the Claims Call Audit Process
Mastering the claims call audit process is essential for maintaining compliance and enhancing service quality in the insurance industry. By systematically reviewing calls, you can identify areas for improvement and ensure that agents adhere to established guidelines. The process involves selecting relevant calls, leveraging transcript tools, and analyzing compliance with regulatory standards.
Effective audits not only reveal compliance issues but also serve as valuable training opportunities. By addressing the findings from these audits, organizations can refine their practices and foster a culture of continuous improvement. Ultimately, mastering this process leads to enhanced performance, greater customer satisfaction, and a more reputable business overall.