How Call Analytics Uncovers Voice of the Customer in Insurance
-
Bella Williams
- 10 min read
In the insurance industry, customer satisfaction is no longer a nice-to-have—it’s a defining competitive edge. Whether in health, auto, or life insurance, policyholders are demanding faster claims processing, clearer communication, and personalized service. Listening to the Voice of the Customer (VoC) is how insurers stay ahead. But true listening doesn’t happen just through surveys or ratings. It happens in real-time conversations. This is why leading insurers are turning to call analytics to extract rich, actionable insights from every customer interaction.
Analyze & Evaluate Calls. At Scale.
What Is Voice of the Customer in Insurance?
Voice of the Customer in insurance refers to structured efforts to capture and understand the experiences, expectations, and frustrations of policyholders across the insurance journey. While digital feedback tools play a role, the most honest and detailed customer insights come from one place: their phone calls.
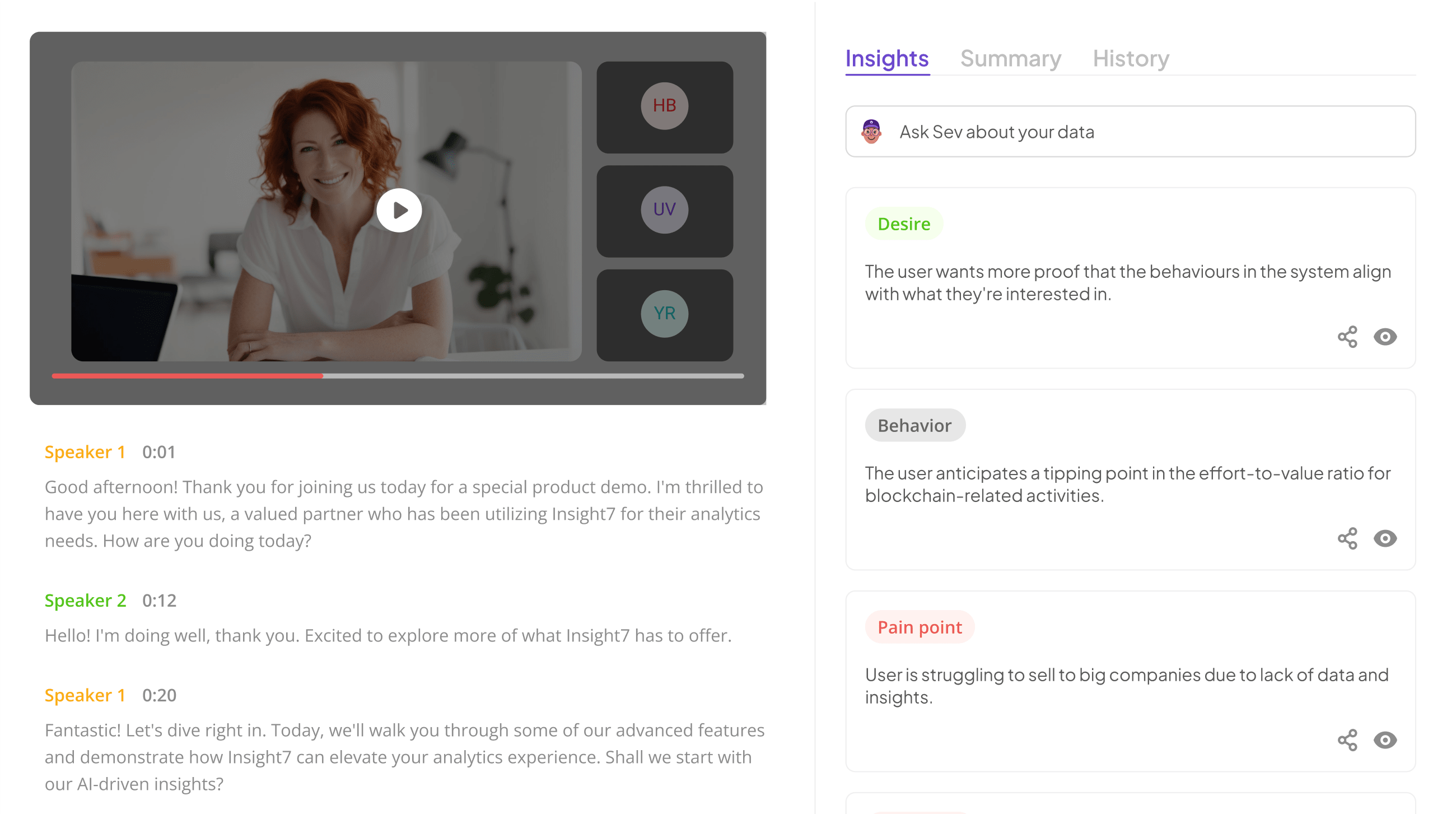
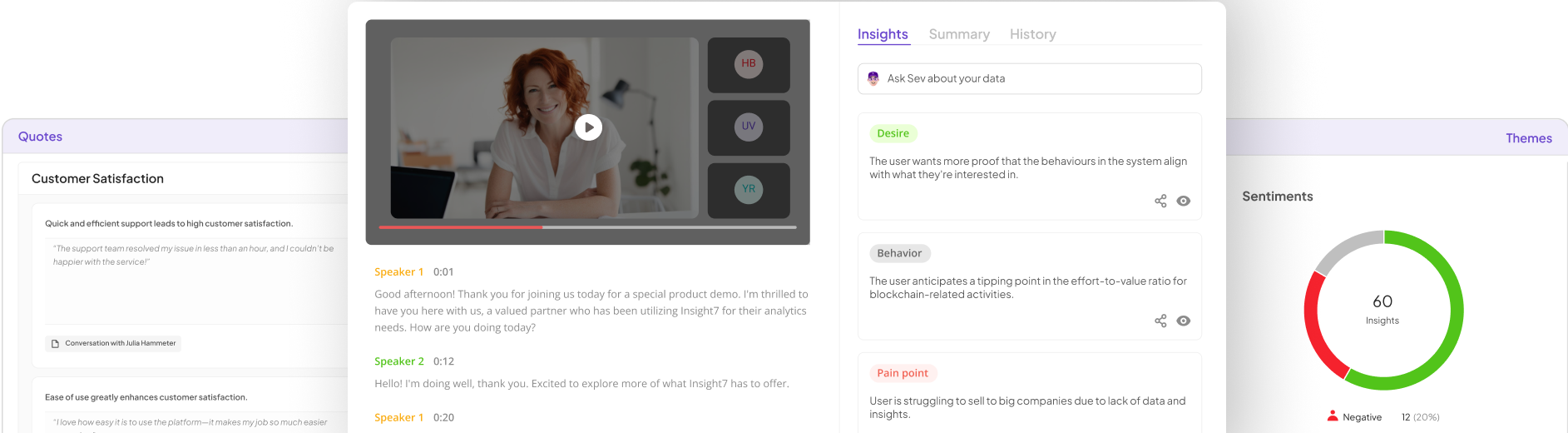
Phone conversations contain rich emotional and contextual signals—especially in insurance, where customers often reach out during stressful life events. VoC via call analytics allows companies to listen at scale, using speech-to-text transcription, sentiment analysis, and keyword recognition to extract themes and emotional cues from every call.
Rather than relying on occasional survey responses, insurers can now tap into the unfiltered voice of their customers, analyze every interaction, and uncover recurring issues affecting claims, renewals, underwriting, and customer service.
Why Call Analytics Is Crucial to Insurance VoC Programs
Call analytics allows insurers to bridge the gap between customer expectations and internal processes. Unlike surveys or emails, phone calls reveal how customers actually feel and what they struggle with at the moment of interaction.
When a policyholder calls about a denied claim or unclear coverage, their tone, word choice, and emotional language give you far more context than a checkbox survey ever could. By analyzing these calls, insurers can detect patterns such as repeated questions, escalation risks, and breakdowns in the claims journey.
This shift from manual call sampling to full-scale, AI-driven analysis enables insurers to listen systematically, act faster, and fix the root causes of dissatisfaction across the business.
Insurance-Specific Pain Points Uncovered Through Call Analytics
The insurance industry presents unique challenges that often result in policyholder confusion or frustration. By analyzing customer conversations in real time, insurers gain visibility into the most common and most damaging pain points.
Claims Delays and Process Breakdown
One of the most emotionally charged interactions happens during the claims process. When customers call to ask why their claim is taking too long, or why a payout was denied, it often stems from unclear communication or unmet expectations.
Call analytics can detect patterns in these calls, such as frequent confusion about required documentation, delays in status updates, or misaligned messaging from agents. Identifying these themes helps claims teams tighten workflows and improve proactive communication, reducing repeat calls and escalating dissatisfaction.
Confusing Policy Language and Coverage Misunderstanding
Insurance policies are filled with legal terminology and fine print. Customers routinely call asking for clarification on what their plan covers. If analytics reveals that customers often question the same clause, rider, or term, it signals a need for clearer documentation and better onboarding.
This insight allows insurers to rewrite complex language, adjust agent scripts, or enhance digital FAQs—reducing dependency on agents and improving self-service clarity.
Long Hold Times and Repeat Contacts
Policyholders calling to make updates or request information often face long wait times, or they’re transferred multiple times between departments. This damages trust, especially when an issue could have been resolved on the first call.
Call analytics tools can flag excessive hold times, repeat callers, or unresolved outcomes. By studying these patterns, contact center managers can reassign resources, improve agent training, and eliminate repetitive friction.
Emotional Frustration Around Renewals and Billing
Renewal periods and billing cycles trigger an influx of calls—many from customers frustrated by unexpected premium hikes or errors in payment processing. These interactions are often laced with emotion.
Sentiment analysis identifies where in the call flow policyholders begin expressing anger, confusion, or dissatisfaction. Insurers can then preemptively adjust their communication around renewals or simplify payment portals to reduce stress and negative sentiment.
At-Risk Policyholders Considering Cancellation
Some of the most valuable insights come from customers who hint at leaving. Phrases like “I’m thinking of switching” or “This is too much hassle” are early indicators of churn risk.
Call analytics surfaces these cancellation signals early—allowing retention teams to intervene with empathy, clarify misunderstandings, or offer tailored incentives to keep the customer onboard.
How Call Analytics Works in the Insurance Contact Center
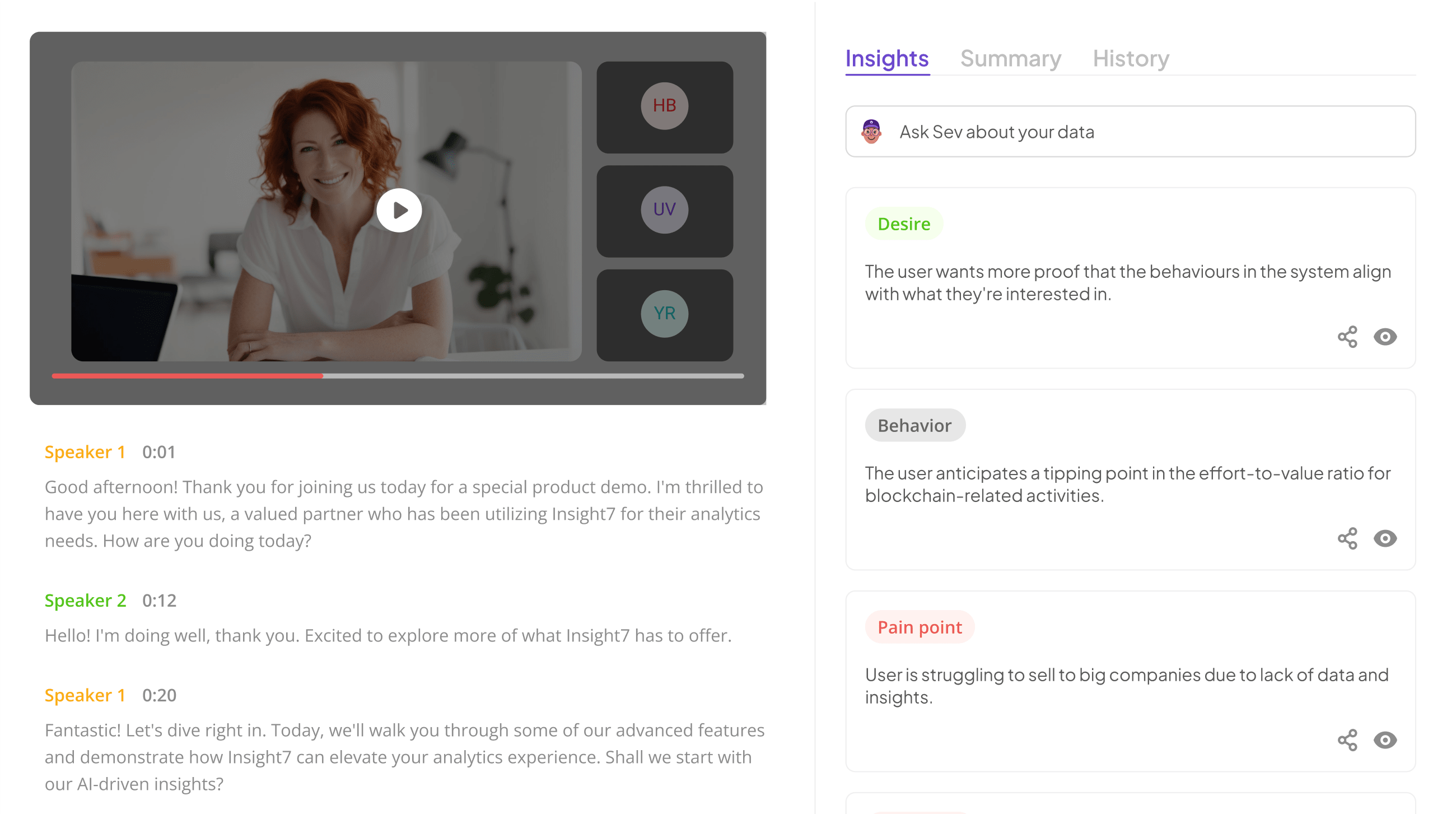
Modern call analytics platforms combine artificial intelligence with insurance domain knowledge to extract meaningful insights from voice data. Here’s how it typically works:
When a call is received, it is automatically transcribed using speech-to-text technology. The resulting text is then analyzed using Natural Language Processing (NLP) and sentiment analysis to detect tone, emotion, topics, and intent. This allows teams to identify:
Which policy terms are most confusing
Which agents fail to resolve issues
When customers express distress or anger
How often specific claim issues arise
Where escalation risks appear across calls
Rather than reviewing a random 2% of calls, insurers now analyze 100% of conversations in real time turning each call into a data point that feeds into continuous improvement.
From Insight to Outcomes: What Call Analytics Improves
Call analytics doesn’t just uncover problems—it enables measurable improvements across the entire insurance value chain. When insurers listen to every customer interaction, they can:
- Improve First Call Resolution (FCR) by ensuring agents are equipped to resolve more inquiries on the first attempt
- Reduce claim cycle time by identifying breakdowns in communication or documentation
- Increase customer satisfaction (CSAT) by proactively addressing repeat call triggers
- Detect early churn indicators and launch targeted retention strategies
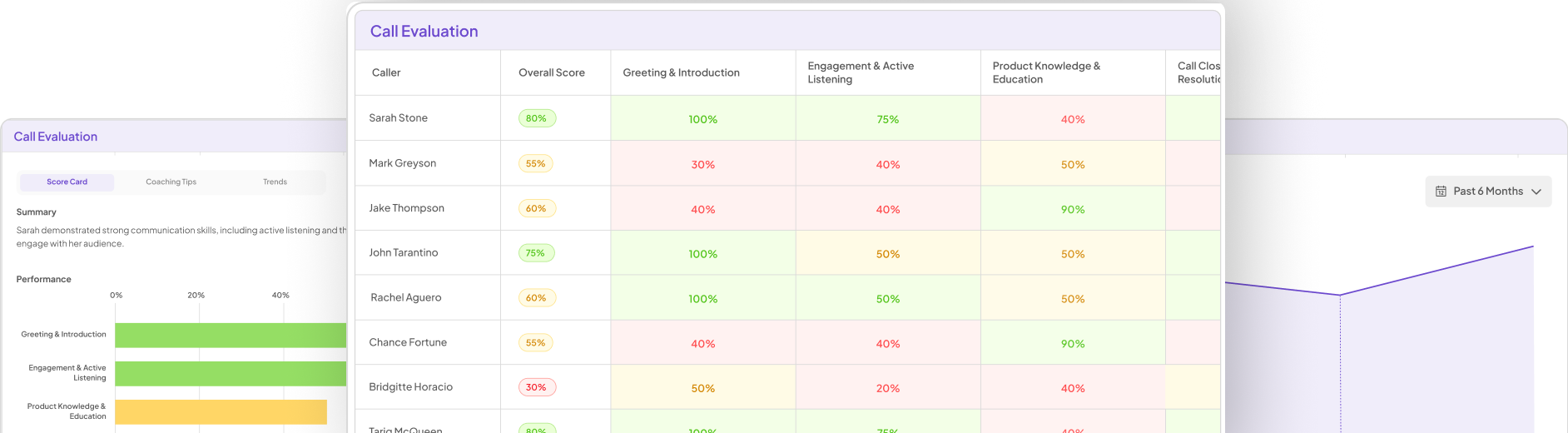
- Strengthen agent performance with real examples from successful and unsuccessful calls
- Enhance compliance by monitoring how well agents deliver required disclosures
By translating qualitative voice data into actionable metrics, insurers gain a competitive edge built on responsiveness, empathy, and efficiency.
How to Successfully Implement VoC Call Analytics in Insurance
To realize the full value of voice analytics in insurance, organizations should start with a structured plan.
Begin by identifying one area of the business with high call volume and high emotional impact—such as claims or renewals. From there, ensure you have the right tools that can accurately transcribe, analyze, and report on calls in your specific domain.
VoC insights must also be shared across silos. Claims, underwriting, CX, product development, and compliance all benefit from understanding what customers are saying and feeling. Create centralized dashboards and use cross-functional teams to act on insights.
Finally, use VoC data not only to fix current problems but to prevent future ones. Trends in call topics can guide improvements in digital tools, training programs, policy language, and even product design.
Addressing Data Privacy and Trust in Voice Analytics
Using customer voice data responsibly is essential in insurance. All call analytics programs should begin with clear customer disclosures—informing callers that their conversation may be recorded and analyzed.
Insurers must ensure that voice data is encrypted, anonymized where appropriate, and stored in compliance with industry regulations. Models should be evaluated regularly to prevent bias and ensure that sentiment detection works across accents and speaking styles.
When implemented with transparency and care, call analytics reinforces customer trust—not just in service, but in the insurer’s commitment to listening.
Conclusion
Voice of the Customer is more than a buzzword in the insurance world. It’s a business-critical tool for understanding what your policyholders are truly experiencing. With call analytics, insurers gain a unique ability to listen at scale, act with precision, and resolve root causes before they damage relationships. For insurers focused on long-term loyalty, real-time feedback, and operational excellence, the path forward is clear: start by listening to your customers and let call analytics lead the way.
Frequently Asked Questions (FAQ)
Q-1: Importance of voice of the customer in Insurance?
A: Voice of the customer in insurance helps identify customer needs, improve service, reduce churn, and drive loyalty through actionable feedback.
Q-2: How can call analytics improve customer satisfaction in insurance?
A: By identifying and addressing customer pain points through call analytics, insurance companies can tailor their services to meet client needs, leading to higher satisfaction levels.
Q-3: What are the key benefits of using call analytics in the insurance industry?
A: Key benefits include enhanced customer satisfaction, informed decision-making, increased customer retention, competitive advantage, and improved operational efficiency.
Analyze & Evaluate Calls. At Scale.